|
|
Posted By Columbus Medical Association - CMA,
Thursday, July 10, 2025
|

Pina Patel, MD, joined the CMA Board of Directors in June 2025. Dr. Patel, practices hospital and palliative care at OhioHealth Physician Group. She is also a member of the Physician Leadership Academy Class of ’25!
What inspired you to pursue a career in medicine?
I have always been drawn to medicine because it is a fascinating intersection between science and the art of healing. It not only improves the lives of individuals that we encounter, but it is also transforming for society. International health work was always my first love and is something I hope to return to someday. I have volunteered in South Africa, the Dominican Republic, Haiti, Mexico, and India—every journey has been rewarding and has grounded me in a way that few things can.
What brought you to Columbus, and what do you enjoy most about practicing here?
My family moved to Ohio from New Jersey back when Columbus Southern Power was acquired by American Electric Power (1984). I have grown up in the Worthington School system and my parents still live in the same home in Powell, Ohio. I left Ohio to train at Mass General Brigham in Boston and then started work as an attending in the San Francisco Bay Area for Kaiser Permanente. Living on both coasts was exhilarating, but nothing compares to my hometown of Powell, Ohio. I have deep roots here and can’t imagine leaving.
What are your areas of clinical/professional interest?
My specialty is Hospice and Palliative Medicine, and given the changing financial landscape of healthcare, I am interested in educating patients on how to access the best palliative and hospice care possible. I have also recently become interested in developing more women physician leaders in corporate healthcare. There remains a lot of work to be done, but when I see the potential of my colleagues and myself, I know there is hope for the future.
What’s one thing you’d like your colleagues to know about you or your work?
I work in the world’s most amazing Inpatient Hospice Unit, Kobacker House. It is part of OhioHealth’s HomeReach Hospice—it was the third freestanding Inpatient Hospice Unit in the country and built by visionaries and pioneers in the field of Palliative Medicine. I am very fortunate to work there and be part of its story.
What’s your favorite restaurant in Columbus?
Veritas. They rotate through global tasting menus, and I am always excited to see their latest creation. My husband and I are foodies!
When you’re not working, how do you like to spend your free time?
I love learning about anything related to history. his could mean through traveling, reading, going to museums, or watching films. I am trying to instill this interest in my children, and I think it’s working.
What’s a fun fact about you that people might not know?
I am fluent in Spanish. I studied for a semester abroad in Spain when I was 16. I lived with a host family with whom I have kept in touch through the years. This summer, after 30 years, I returned to Spain with my own family and reunited with my host-parents. It was a very moving experience. My 90-year-old host father greeted me while wearing the same apron I wore when I would help him cook paella.
If you could have dinner with any historical or medical figure, who would it be and why?
I am so fascinated by history that this is a very hard question to answer. British history, especially during the War of the Roses and the Tudor Dynasty, has always been so engaging for me. If I were pressed on it, I would say I would love to meet Queen Elizabeth I. She was a survivor of unending political intrigue. As queen, she did not mention her mother (the legendary Anne Boleyn), but upon her death it was found she was always wearing a locket ring that contained portraits of her and her mother.
What’s the best piece of advice you’ve ever received?
Treat yourself with kindness. Frame a picture of yourself as child and keep it close at hand. When you view it, give yourself the same grace now that you would give yourself as a child. Ask yourself: Knowing what I know now, what would you tell the child you once were?
Tags:
Board of Directors
Board Spotlight
Physicians Leadership Academy
PLA
Permalink
| Comments (0)
|
|
|
Posted By Tracy Davidson, CEO,
Thursday, July 10, 2025
|

At the Columbus Medical Association and Affiliates (CMAA), we believe learning is more than just a stage in life — it’s a mindset. It doesn’t end when you graduate or put on your white coat. The drive to continue learning lays the foundation for strong leadership, sparks innovation, and bridges generations of healthcare professionals. That’s why this summer, we’ve embraced continuous learning not only as something we provide — but as something we live, grow through, and celebrate together.
In my May message, I shared that our organization had begun a journey to evolve — to remain a vital, trusted partner to our physicians and the broader community. We started by engaging a new public policy partner, who has already provided invaluable insights during these turbulent times. We also partnered with Dr. Mrunal Shah to learn directly from our physician members and ensure your voice is heard. He has held a number of one-on-one and group meetings and shared meaningful feedback. Stay tuned for more opportunities to share your perspective.
On June 30, we kicked off the next phase of this journey with our first visioning session with Just Bloom, an award-winning organization specializing in creativity and leadership development. CMAA staff, physician Board members across the affiliates, as well as community Board participants came together for a thought-provoking workshop designed to expand how we think, lead, and collaborate. These sessions will continue to guide us — using science-backed methods — to unearth a vision that both modernizes and honors our legacy.
That same spirit of lifelong learning was reflected on June 26, as we celebrated 17 physicians graduating from the Physicians Leadership Academy (PLA). These individuals dedicated nine months to personal growth, reflection, and peer learning — emerging with tools to lead with intention and compassion.
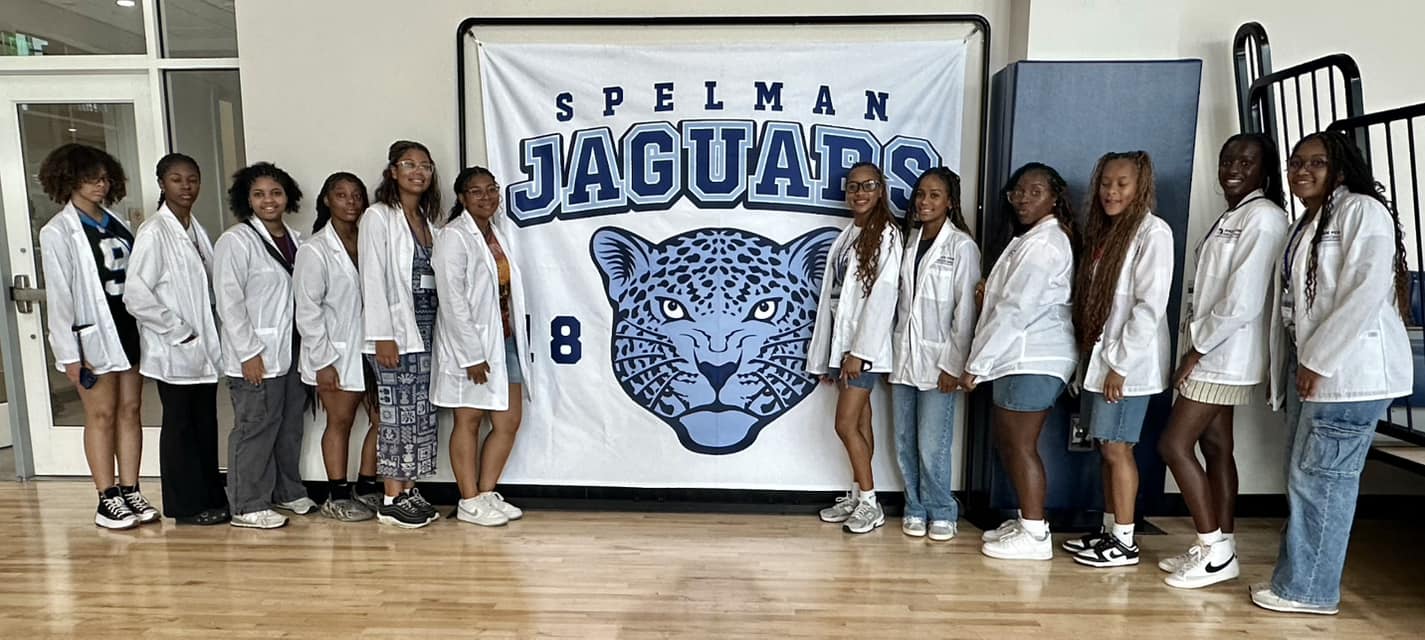
Education also drives our work with the next generation. Our Made for Medicine students took their learning on the road in June, embarking on our first-ever HBCU Medical School and College Tour. Fifteen students traveled to Nashville and Atlanta, visiting historically Black colleges, universities, and medical schools — and connecting with professionals who reflected their aspirations. It was more than a tour — it was a transformative experience rooted in representation, access, and belief in their potential.
We continue to be inspired by the CMA Foundation’s Youth Advisory Council, a student-led body of 13- to 18-year-olds learning the ins and outs of philanthropy and grantmaking. These young leaders are gaining firsthand experience in how community investment can shape health and equity for years to come.
Our commitment to education and growth extends to medical school. We’re especially excited about our upcoming CMA Medical Student Specialty Fair this October. By polling medical students about their interests and inviting physician members to share their stories and insights, we’re creating a meaningful, two-way exchange that connects curiosity with experience.
Our CMA Practice Managers Group continues to convene for educational sessions that provide real-world value. These gatherings have featured several of our strategic partners in legal and communications — all collaborating to support physician practices across Central Ohio.
While COTS leaders continue to champion life-saving disaster preparedness funding, they also remain focused on what they do best: preparing our emergency responders to act swiftly and save lives. Find out more about their educational offerings here.
As we continue the essential work of planning for the future of our organization, we never lose sight of the day-to-day value CMA provides: empowering physician, supporting practices, and nurturing growth at every stage.
Learning will remain a constant in everything we do — not just because it prepares us for tomorrow, but because it brings us together today.
Tags:
CMA Foundation
CMA Practice Managers Group
CMAA
COTS
Education
Made for Medicine
Physicians Leadership Academy
PLA
Youth Advisory Council
Permalink
| Comments (0)
|
|
|
Posted By Columbus Medical Association - CMA,
Thursday, July 10, 2025
|

From June 22–26, 2025, Made for Medicine embarked on its first-ever HBCU Medical School and College Tour. Fifteen Phase III students participated in this five-day, four-night experience, traveling to historically Black colleges, universities, and medical schools in Nashville, Tennessee, and Atlanta, Georgia.
The tour featured a full daytime itinerary, including visits to Fisk University, Vanderbilt University, Meharry Medical College, Tennessee State University, Morehouse School of Medicine, Morehouse College, and Spelman College. In the evenings, students bonded through games, museum visits, and meaningful conversations and connections with current Black physicians in Atlanta.
A standout moment of the trip was a private meeting with Former U.S. Ambassador to the United Nations and civil rights icon Andrew Young. At 93 years-old, Ambassador Young shared inspiring words of wisdom and encouragement with our future physicians. He was joined by Calvin Smyre, longtime member of the Georgia House of Representatives, in the very building that bears his name—the Calvin Smyre Education Conference Center.
This once-in-a-lifetime opportunity was made possible through the efforts of Mr. Eugene Duffy, a Morehouse alum and the uncle of Dr. Laura Espy-Bell. We are incredibly grateful for his role in creating such a memorable experience.
Looking ahead, Made for Medicine hopes to offer this tour biennially, for our high school aged students. By introducing them early to the rich academic and cultural offerings of HBCUs and medical schools, we aim to inspire and support the next generation on their journey to becoming physicians.
Learn more about Made for Medicine on our website.



Tags:
Made for Medicine
Permalink
| Comments (0)
|
|
|
Posted By Columbus Medical Association - CMA,
Thursday, June 26, 2025
|

CMA’s Practice Managers group gathered for their monthly meeting on June 18, 2025, for a workshop designed to elevate their designs and ensure their communications are accessible to all.
From creating polished visuals to free resources to assist those with visual impairments, Barb Burgie and Melanie Farkas of Burgie MediaFusion shared practical tools and creative insights. The group had a great discussion on strategies to help them connect with patients and communities.
Thank you to meeting sponsors:
- CMA Foundation – Premier Sponsor
- Point Law
- BMD
- Buckeye Health Plan
- Mag Mutual
Contact Melanie Farkas to request a copy of the meeting slides.
Contact Lynn Manoogian to get involved in the Practice Manager group!
Tags:
Practice Managers
Permalink
| Comments (0)
|
|
|
Posted By Columbus Medical Association - CMA,
Thursday, June 26, 2025
|

Made for Medicine students and faculty had a whirlwind tour of medical schools and colleges this week. Founder and president, Laura Espy-Bell, MD, along with several other faculty members, took more than a dozen students to prestigious medical schools and historically Black colleges in Tennessee at Atlanta. They visited:
- Fisk University, Nashville, TN
- Meharry Medical College, Nashville, TN
- Tennessee State University, Nashville, TN
- Morehouse College, Atlanta, GA
- Spelman College, Atlanta, GA
During the trip, the group also visited the Tennessee State Museum and Children’s Healthcare of Atlanta. The tour is meant to provide firsthand exposure to students interested in pursuing careers in medicine.
“As we continue to guide them on their journey as future doctors, it’s important they understand the historical significance of Black people in medicine as well as the institutions who have supported and shaped the journey,” said Dr. Espy-Bell.
Check out photos from the trip on Made for Medicine’s Instagram page. Learn more about Made for Medicine here.
Tags:
Made for Medicine
Permalink
| Comments (0)
|
|